Public and Community Health: Building Stronger, Healthier Neighborhoods Together
Understand public and community health
Public and community health represent interconnect approaches to improve population well bee. While public health typically operate at broader governmental and institutional levels, community health focus on neighborhood specific needs and solutions. Unitedly, they form a comprehensive framework for address health challenges through prevention, education, and collaborative action.
The distinction between these approaches matters. Public health initiatives frequently implement all-encompassing reach policies and programs, while community health efforts tailor interventions to local contexts. This complementary relationship allows for both systemic change and culturally responsive solutions.
The core principles of community health
Community health operate on several fundamental principles that distinguish it from traditional medical models:
Prevention over treatment
Instead than focus solely on treat illness, community health emphasize prevent health problems before they develop. This approach include promote healthy behaviors, reduce environmental hazards, and address social determinants of health.
Preventive strategies might include vaccination campaigns, nutrition education programs, or community fitness initiatives. These efforts not but improve quality of life but besides reduce healthcare costs in the long term.
Equity and access
Health disparities persist across different populations base on factors like race, income, geography, and education. Community health programs work to identify and eliminate these inequities by improve access to resources and services.
This principle manifest through mobile health clinics serve remote areas, multilingual health education materials, or slide scale payment options at community health centers. The goal remain consistent: ensure everyone have a fair opportunity to achieve optimal health.
Community participation
Effective community health initiatives involve residents in planning, implement, and evaluate programs. This participatory approach ensure interventions address actual community need instead than perceive problems.
Community health workers oftentimes serve as bridges between formal healthcare systems and neighborhood residents. These trust individuals share cultural backgrounds with the communities they serve, facilitate more effective communication and trust building.
Social determinants of health
The conditions in which people live, work, learn, and play importantly impact their health outcomes. These social determinants include:
Economic stability
Income levels, employment opportunities, and financial security straightaway affect health. Communities with high unemployment or poverty rates typically experience worse health outcomes than more affluent neighborhoods.
Public and community health initiatives address economic factors might include job training programs, affordable housing initiatives, or policies support living wages. These upstream interventions create environments where healthy choices become more accessible.
Education access and quality
Educational attainment correlate powerfully with health outcomes. Higher education levels broadly predict better health, while limited educational opportunities frequently accompany poorer health status.
School base health centers, adult literacy programs, and early childhood education initiatives represent community health approaches to improve educational determinants. These programs recognize that learning and health reinforce each other throughout life.
Neighborhood and built environment
Physical surroundings deeply influence health behaviors and outcomes. Safe parks encourage physical activity, while food deserts limit access to nutritious options. Environmental hazards like air pollution disproportionately affect disadvantaged communities.
Community health initiatives might address these factors through community gardens, pedestrian friendly infrastructure improvements, or advocacy for environmental justice. These efforts transform neighborhoods into places that support instead than hinder health.
Successful models in community health
Community health centers
Federally qualified health centers (fFCS) )ovide comprehensive primary care services disregarding of patients’ ability to pay. These centers typically offer medical, dental, and behavioral health services under one roof, remove barriers to integrate care.
Beyond clinical services, many community health centers coordinate outreach programs, conduct health screenings, and connect patients with social services. This holistic approach address multiple health determinants simultaneously.
Collective impact initiatives
Complex health challenges require coordinate responses across multiple sectors. Collective impact models bring unitedly healthcare providers, schools, businesses, government agencies, and community organizations around share goals.
These collaborations establish common metrics, coordinate activities, and maintain continuous communication. Examples include initiatives address childhood obesity, substance use disorders, or maternal health disparities. The power lie in align diverse resources toward unified objectives.
Community health need assessments
Effective community health planning begin with understand current needs and assets. Community health need assessments (cCNAs))ombine quantitative data analysis with qualitative community input to identify priority issues.
Hospitals, public health departments, and community organizations frequently collaborate on these assessments, create share understanding of local health challenges. The result implementation strategies guide resource allocation and program development base on identify priorities.
Public health infrastructure
While community health focus on neighborhood level action, public health provide essential infrastructure support these local efforts:
Surveillance systems
Public health departments collect and analyze data on disease patterns, health behaviors, and population demographics. This surveillance helps identify emerge threats and evaluate intervention effectiveness.
During disease outbreaks, these systems become specially crucial for track cases, identify risk factors, and guide response efforts. The COVID-19 pandemic highlight both strengths and weaknesses in current surveillance capabilities.

Source: blogs.dal.ca
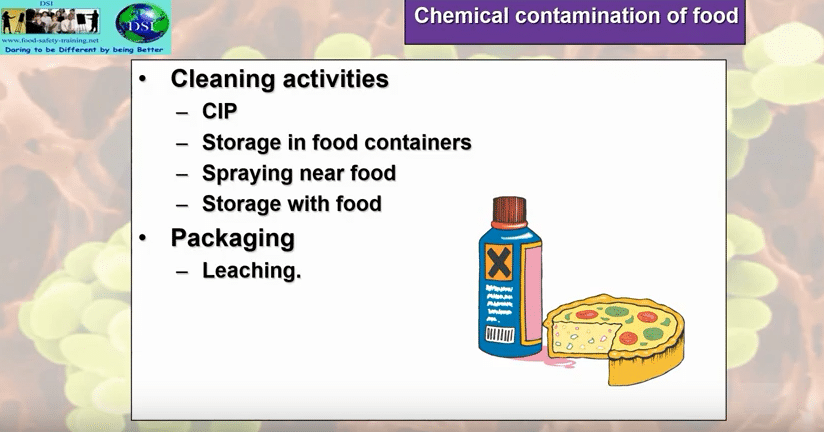
Laboratory networks
Public health laboratories perform specialized testing for infectious diseases, environmental contaminants, and other health threats. These facilities support both routine monitoring and emergency response activities.

Source: dailypublic.com
The connection between public health labs and community health become evident during water quality crises, foodborne illness outbreaks, or emerge infectious diseases. Their technical capabilities complement community base prevention efforts.
Emergency preparedness
Public health agencies coordinate planning for disasters, disease outbreaks, and other health emergencies. These preparedness efforts include train healthcare workers, stockpile supplies, and develop communication protocols.
Community health organizations oftentimes participate in these planning processes, ensure emergency responses account for local needs and vulnerabilities. This collaboration prove particularly important for reach marginalize populations during crises.
Current challenges in public and community health
Funding sustainability
Many community health initiatives rely on grant funding with limited timeframes. This creates challenges for long term planning and program sustainability. When funding end, yet successful programs may disappear despite continue community need.
Innovative financing models like wellness trusts, social impact bonds, and braid funding streams offer potential solutions. These approaches diversify revenue sources and create more sustainable funding mechanisms for community health work.
Workforce development
The public and community health workforce face significant challenges, include shortages in key roles, limited diversity, and inadequate training opportunities. Rural and underserved areas peculiarly struggle to recruit and retain qualified professionals.
Address these challenges require investments in education pipelines, competitive compensation, and supportive work environments. Community health worker certification programs, loan forgiveness initiatives, and mentorship opportunities represent promising strategies.
Technology integration
While technological advances offer tremendous potential for improve community health, implementation barriers persist. Digital divide limit access among vulnerable populations, interoperability issues hinder data sharing, and privacy concerns raise ethical questions.
Successful technology integration require address these challenges through community center design, digital literacy programs, and thoughtful policies. When implement efficaciously, tools like telehealth, mobile health applications, and electronic health records can extend the reach of community health initiatives.
The future of community health
Value base care models
Healthcare payment systems progressively reward outcomes kinda than service volume. This shift creates new opportunities for community health approaches that address root causes and social determinants.
Accountable care organizations, patient center medical homes, and other value base models progressively incorporate community health workers, social service referrals, and prevention programs. This integration recognizes that meaningful health improvement require address factors beyond clinical care.
Cross sector partnerships
The future of community health depend on stronger connections across traditionally separate sectors. Housing agencies, transportation departments, education systems, and healthcare providers progressively recognize their interdependent roles in promote health.
These cross sector partnerships manifest through initiatives like medical legal partnerships address housing conditions, food prescription programs connect healthcare with local agriculture, or school base health services integrate education and healthcare.
Community ownership
Maybe the virtually promising development in community health involve shift power dynamics toward greater community control. This approach recognize that sustainable change require meaningful decision make authority for those virtually effect by health disparities.
Community own models include resident lead health councils, participatory budgeting for health resources, and community land trust develop health promote infrastructure. These approaches build both immediate health improvements and long term community capacity.
Get to involve in community health
For individuals
Community members can contribute to public and community health efforts through various channels:
- Volunteer with local health initiatives or community organizations
- Participate in community health assessments and planning processes
- Advocate for health promote policies at local, state, and federal levels
- Pursue education or careers in public health, community health work, or related fields
- Support community health centers and other local health resources
For organizations
Businesses, faith communities, and other organizations play important roles in community health:
- Implement workplace wellness programs and health supportive policies
- Partner with health initiatives to reach specific populations
- Contribute resources, facilities, or expertise to community health efforts
- Incorporate health considerations into organizational planning and decision-making
- Address social determinants through employment practices, purchase decisions, and community investments
Measure success in community health
Evaluate community health initiatives require look beyond traditional clinical metrics. Comprehensive assessment include:
Health outcomes
While disease rates and health status remain important measures, community health evaluations frequently track additional outcomes like quality of life, functional ability, and self report wellbeing. These measures capture broader impacts on community vitality.
Process measures
How programs operate matters equally often as what they achieve. Process evaluation examine factors like community engagement levels, service accessibility, cultural responsiveness, and partnership function. These indicators help identify implementation strengths and challenges.
Community capacity
Sustainable community health improvement depend on build local capabilities. Evaluation measures might include leadership development, resource mobilization skills, collaborative networks, and community ownership of health initiatives.
The virtually meaningful evaluations incorporate community perspectives throughout the process, from define success metrics to interpret results and planning improvements. This participatory approach ensures evaluation serve learning and growth instead than simply judgment.
Conclusion
Public and community health offer powerful frameworks for address complex health challenges through collaborative, prevention focus approaches. By address social determinants, build community capacity, and integrate diverse perspectives, these approaches create healthier environments where everyone can thrive.
The journey toward healthier communities require sustained commitment from individuals, organizations, and systems work unitedly across traditional boundaries. While challenge persist, innovative models and grow recognition of health’s social dimensions create new opportunities for transformative change.
Finally, public and community health remind us that health emerge not mainly from hospitals or clinics, but from the neighborhoods, relationships, and daily environments where people live their lives. By strengthen these foundations, we build not equitable better health outcomes but more vibrant, equitable, and resilient communities.
MORE FROM eboxgo.com